Save with Insurance Coverage
Use your insurance benefits to save on all of our top-rated wearable pumps.
Check eligibility
USE INSURANCE COVERAGE WITH:

A signed RX from your OBGYN
Insurance information & card

Your OBGYN’s contact information
What to Expect
In just a few easy steps, you can see which breast pumps are covered by your insurance plan. Here's how to get started.
Get Started
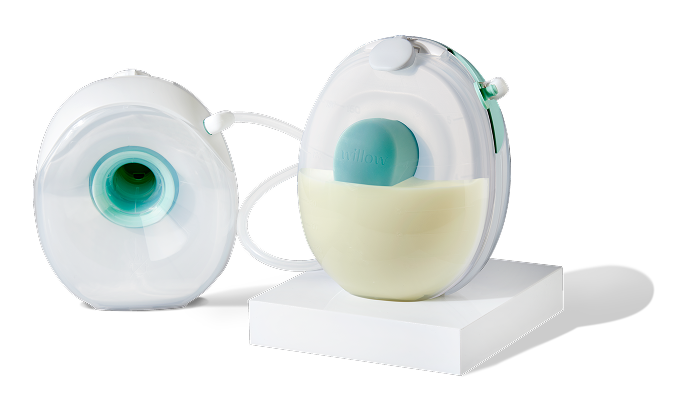
Choose the Willow for you
Here's a quick breakdown of how our pumps compare.
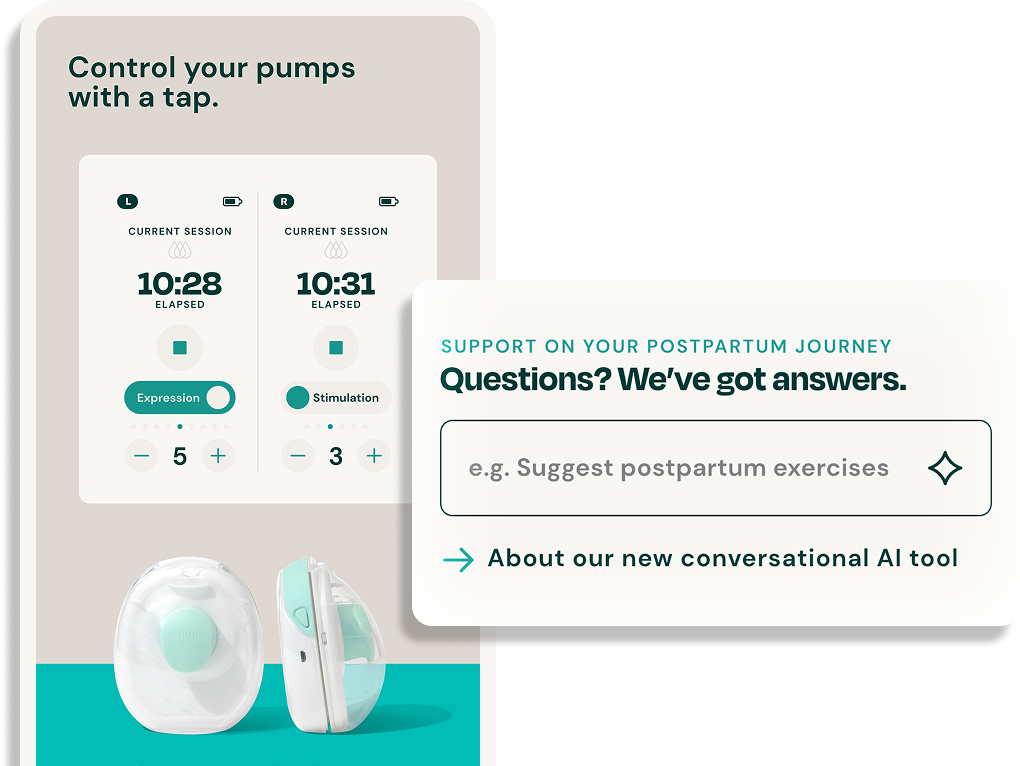
Get access to feeding support with the Willow app
All Willow users have access to the Willow app, which connects moms to our science-backed articles, postpartum resources on feeding and sleeping, and experts such as IBCLCs, pediatricians, and more. It’s also where moms can get instant answers to urgent questions through Ema, our conversational and medically validated AI-tool.
Learn More


Frequently Asked Questions
Will my insurance cover Willow?
Each insurance plan is different in what pump they will cover. We can support your efforts by investigating your insurance benefits through our insurance verification program. There may be out-of-pocket expenses for you in obtaining your Willow Pump, but you may be able to use FSA or HSA dollars to cover these costs. Alternatively, you can contact your insurance company directly to learn more about your options.
What does my prescription need to say?
Your prescription should be written within 90 days of when you order your breast pump, and it should be signed by an MD, CNM or NP. It does not have to say that you are getting a Willow breast pump, but it does need to have the following codes:
Item: E0603 (electric breast pump)
Diagnosis: Z39.1 (post-partum lactation)
If your prescription was not written this way, or was signed too early in your pregnancy, we will need to reach out to your OB for an updated copy.
Why is there a price difference between what your Insurance Verification Program quoted and what my insurance quoted?
Our partner quotes according to their contract with your insurance. Some insurances offer direct reimbursement where members can submit their own claims and be paid back directly. They may also be quoting you rates from a different year than our partner's contract was created so there may haven been changes which do not apply to our partner's contracted rate.
My insurance was not in the drop-down so I chose “Other”. How long will it take to know if my insurance pays?
When you choose a non-contracted insurance plan, we ask that you pay for the pump up front since our partner does not have a contracted rate with your insurer and therefore do not know what they may pay for the pump. However, you will be refunded whatever portion your insurance pays after the billing. We understand you will be waiting anxiously for updates. Out of network billing process can take several weeks to several months depending on your insurance company.
Which questions should I ask my insurance company?
• Does my plan cover an electric breast pump?
• When am I eligible to receive a breast pump through insurance?
Depending on your plan, you may be eligible before the baby is born and/or up to 12 months after delivery.
• Do I have to purchase your In-Network “recommended” breast pump(s) or can I purchase an Out-of-Network pump and get reimbursed?
• What is the dollar limit to coverage? Do I need to hit a deductible first?
If your insurance allows for Out-of-Network, you might need to meet your deductible before they will cover the cost.
• Do I need a prescription and from whom (e.g., pediatrician, OBGYN, nurse practitioner)? What information does it need to include?
If a prescription is required, your physician or midwife can assist you. Willow is not a health care provider and cannot provide a NPI number or diagnosis code. We can provide an itemized invoice which includes our tax ID number, legal company name and address. If you need this information, reach out to our customer care team.
• Do you cover breast pump supplies like flanges, storage bags, etc?
Depending on your plan, some insurance companies will cover part or all of the cost of pumping accessories.
• Are specific reimbursement codes required?
For the Willow Pump and accessories, you may need the following codes*: Pump E0603, Flange A4284, Pump Tube A4281, Milk Bags A4287 and Container A4285. Your insurance company ultimately decides which codes are appropriate.
• Can I purchase a Willow Pump now and provide a receipt for reimbursement?
Check with your insurance. Some companies will allow you to submit a receipt from Willow or another retailer for reimbursement. You can either submit a receipt to your insurance company directly or use our insurance form above and have a claim sent in on your behalf. Do not do both as it may result in the denial of one or both claims.
When will Willow be In-Network with my insurance?
We’re working hard to give moms more options to purchase Willow through insurance.
If you are unhappy with your In-Network options, ask your insurance provider to establish an In-Network contract with Willow–this may help expedite the process
Already purchased your pump and looking for reimbursement?
If you have already purchased a Willow pump and would like to seek reimbursement from your insurance company, contact them directly to determine what specific documentation you need in order to be reimbursed.
Please note, Willow is not a healthcare provider and should not be listed as “Provider” on any reimbursement request.
In the area requesting a HCPCS code for your pump, you should enter E0603 (this is the specific code for an electric breast pump).
Questions to ask your insurer if you have already purchased a pump:
Where can I find the reimbursement request form for my breast pump purchase?
Is the Date of Service the date I received the pump, the date I ordered the pump or my baby’s delivery date?
What specific additional documentation do I need in order to submit this request?
Will my OB be noted as the provider since he/she provided the prescription? If not, what provider information is necessary (note: Willow is not the provider).
Do I need to exclude the sales tax amount I paid from the total to be reimbursed?
Do I have coverage for accessories and resupplies?
Can I use my FSA/HSA to pay for Willow® breast pumps and pump parts?
You can pay for your pump, milk bags, milk container, and pump replacement parts with money from an FSA or HSA. Simply pay with your FSA/HSA debit card at checkout, or pay with another credit card and submit your receipt to your plan's administrator for reimbursement. If you run into any issues, the best thing to do is reach out to your card’s administrator to find out why. FSA or HSA funds are not applicable on products not directly used by your breast pump, such as pumping bras, cases, carrying bags, body care products, etc.
View Our Help Center