Ok, traditionally speaking breastfeeding means feeding a suckling infant directly from the breast. For centuries breastfeeding was an infant feeding practice that only involved suckling at the breast but in modern times breastfeeding fortunately encompasses much more.
Human milk extraction from the breast using mechanical pumps and fed to infants in bottles or cups is becoming increasingly common among lactating people. What you may not know is that these ‘alternative’ ways of providing human milk to babies are endorsed nationally by groups like the American Academy of Pediatrics1 as being on par with feeding milk directly from the breast.
Within the past 10 years, surveys of women in large US-based studies have shown that more than 85 percent ‘pumped’ at least once and about 5 to 10 percent pump for their infant(s) exclusively2. The need for lactating people to work outside the home, advancements to pumping technologies and the normalization of pumping within households, the workplace and society is responsible for the uptick in human milk feeding away from the breast. While this makes a whole lot of sense and it is in my opinion super exciting, we still have so much to learn about ‘alternative’ breastfeeding.
In many respects, feeding an infant directly from the breast might be considered to be a whole lot easier. Just look at this diagram below created by Dr. Kathleen Rasmussen of Cornell University.
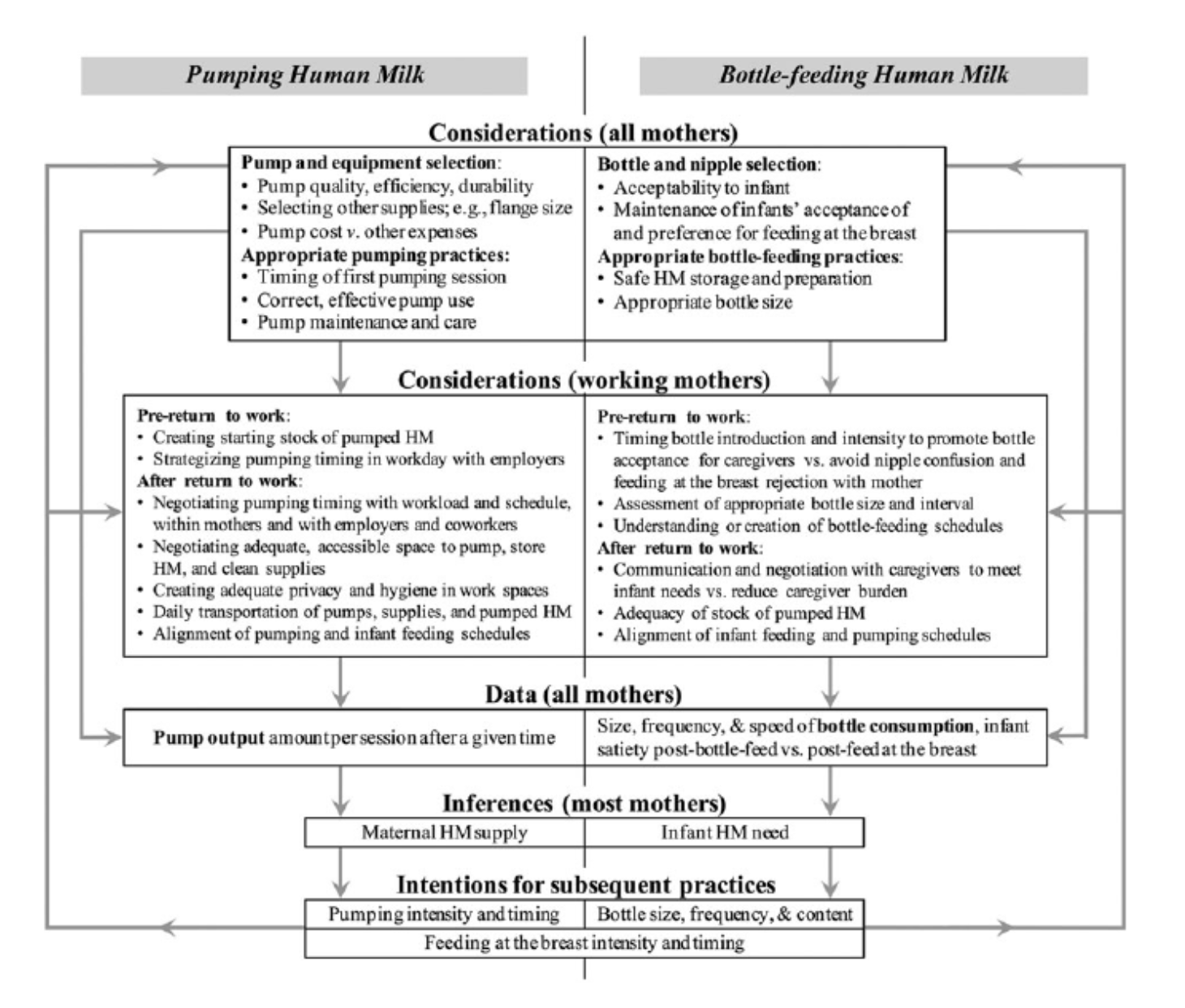
Pumping milk and then feeding human milk in a bottle comes with SO many considerations and ongoing decisions for caregivers. There are decisions around the pump itself like the type and the cost or the flange sizes. Not to mention the considerations for pumping outside the home, how to store the pumped milk and then how to properly feed the milk in a bottle and considerations for nipple confusion, changes to the feeding schedule and feeding cues. Urg!
Yet, despite all these what could be thought of as roadblocks to meeting breastfeeding goals, guess what? In a study of over 3,000 US mothers those who reported pumping between 1.5 and 4.5 months postpartum expressed goals to feed human milk for longer. Yet, interestingly they found that mothers who pumped at all were less likely to be feeding with human milk at 6, 9 and 12 months postpartum. On average they stopped feeding with human milk about 6 weeks prior to mothers who did not pump at all. And the more the mother pumped, the sooner she was likely to stop feeding human milk altogether.
So what we know from this study is that Moms who pump are WANTING to feed their babies human milk for longer. But they also have to return to work. So you can see the juxaposition here: if a woman who returns to work wants to follow the recommended timelines for feeding human milk AND return to her job, she has to find another way to feed her baby. Can she take her baby to work? Probably not—we don't have onsite child care readily available in this country. Can she take longer maternity leave? That's not an option for most women either. You can see where I'm headed here. She has to pump to provide for her baby, but then something happens. She misses pumping sessions to meet her demands at work and she starts to second guess everything - is my baby getting enough? Am I producing enough? And so forth.
So as I read this paper, I was shaking my head. I was shaking my head because healthcare providers, scientists, lactation consultants and many of you are striving to better support mothers in choosing human milk as the main source of nourishment for their child. To ensure more babies receive human milk and for longer, pumping IS necessary to achieve this goal. Many American mothers are in the workforce and, rely on pumping to provide human milk after returning to work. We need more research to better understand a woman’s relationship with her pump and her reasons and motivation for pumping, the challenges with pumping and her reasons for stopping. We also need research to better understand how we need to support mothers who need to pumping and from the perspective of the infant we need to continue to learn the benefits of human milk for growth and development.
To all reading this post, this is a call to action for research of non-traditional infant feeding practices and to lock arms with one another in support of a lactation journey that meets your personal goals and desires.
Sources:
- Section on Breastfeeding. Breastfeeding and the use of human milk. Pediatrics 2012;129:e827–41.
- Labiner-Wolfe J, Fein SB, Shealy KR, Wang C. Prevalence of breast milk expression and associated factors. Pediatrics 2008;122(Suppl 2):S63–8.
- Felice JP, Geraghty SR, Quaglieri CW, Yamada R, Wong AJ, Rasmussen KM. “Breastfeeding” but not at the breast: Mothers' descriptions of providing pumped human milk to their infants via other containers and caregivers. Matern Child Nutr. 2017;13:e12425.

















